At Spark Healthcare, we understand the complex relationship between bipolar medication and weight management. Many individuals with bipolar disorder face challenges in maintaining a healthy weight while on their prescribed medications.
This blog post explores the effects of common bipolar medications on weight and provides practical strategies for managing weight fluctuations. We’ll also delve into the psychological factors that influence weight management in bipolar patients and discuss how to achieve a balanced approach to treatment and overall well-being.
How Bipolar Medications Impact Weight
Mood Stabilizers: A Mixed Picture
Lithium, a common mood stabilizer, has long been associated with weight gain. However, recent research challenges this notion. A 2022 meta-analysis found that lithium doesn’t significantly impact body weight in people with bipolar disorder. The average weight increase was just 0.462 kg, which wasn’t statistically significant.
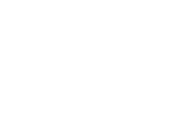
Valproic acid, another mood stabilizer, is more likely to cause weight gain. Studies show that up to 70% of patients taking valproic acid experience weight gain, with an average increase of 5-10 kg over the first year of treatment.
Antipsychotics: Potential for Significant Weight Gain
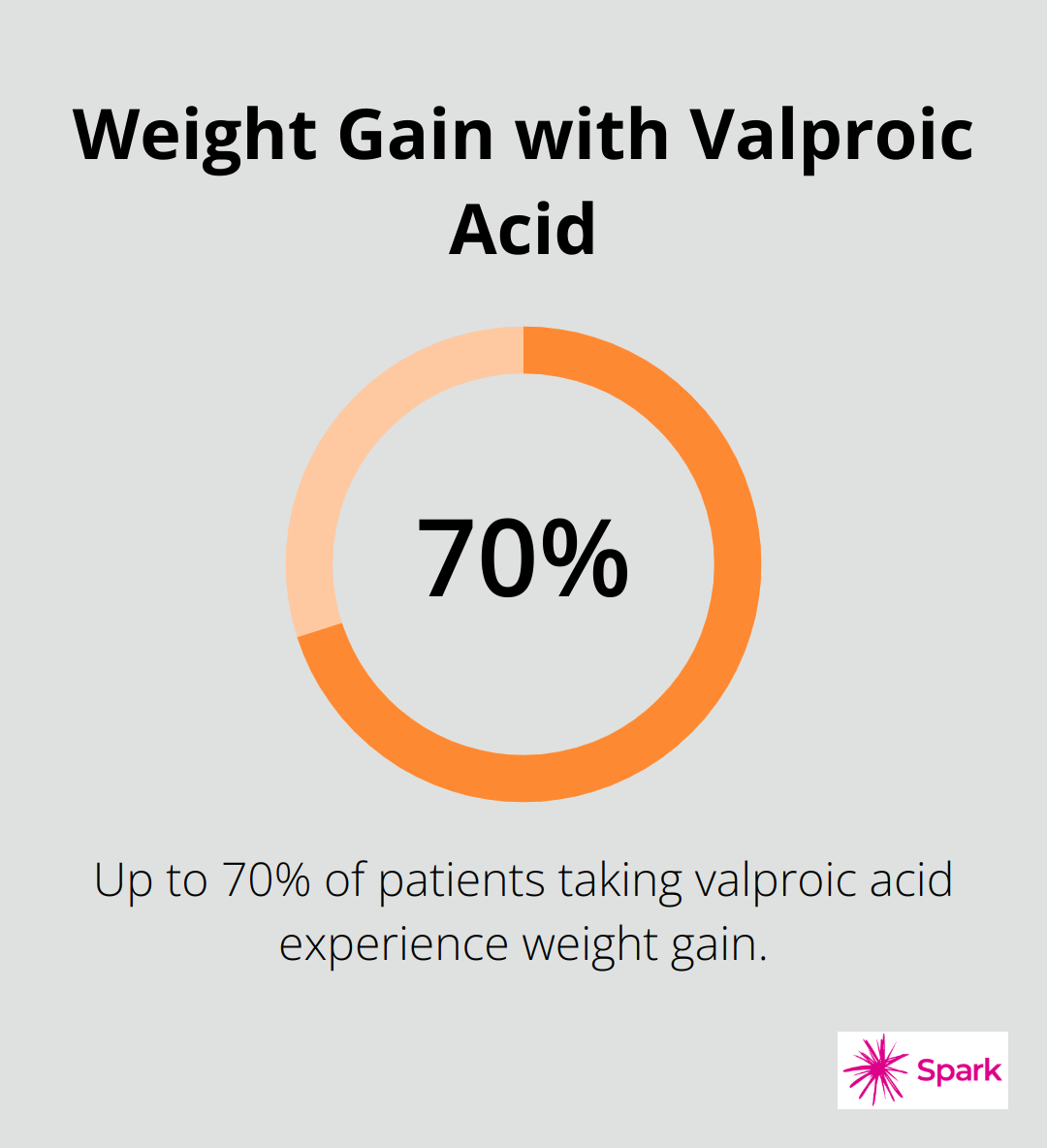
Antipsychotics, particularly second-generation or atypical antipsychotics, are known for their weight gain potential. Olanzapine and quetiapine are among the most likely to cause significant weight gain.
A study found that patients taking olanzapine gained an average of 4.15 kg over 10 weeks. Quetiapine caused an average weight gain of 2.1 kg over the same period.
Antidepressants: Varied Effects on Weight
The impact of antidepressants on weight varies. Some, like fluoxetine (Prozac), are generally weight-neutral or may even cause slight weight loss in the short term. Bupropion (Wellbutrin) is known for its weight loss effects and is more likely to cause weight loss than gain.
Understanding the Mechanisms
The mechanisms behind medication-induced weight changes are complex. Some medications increase appetite, particularly for high-calorie foods. Others may slow metabolism or alter how the body processes and stores fat.
For instance, olanzapine increases levels of ghrelin (a hormone that stimulates appetite). It also affects insulin sensitivity, potentially leading to increased fat storage.
Telehealth services make it easy for patients to regularly check in and discuss any concerns about medication side effects. This proactive approach allows for timely adjustments to treatment plans, helping patients manage their weight more effectively while still receiving bipolar medication.
As we move forward, it’s important to consider strategies for managing weight while on bipolar medication. These strategies can help patients maintain their health and well-being without compromising their mental health treatment.
How to Manage Weight on Bipolar Medication
Regular Monitoring and Open Communication
Tracking your weight weekly is essential. Many patients find that a digital scale and a weight tracking app help them identify trends early. Share this data with your healthcare provider during regular check-ins.
Don’t wait for your next scheduled appointment if you notice rapid weight changes. Most healthcare providers offer easy ways to reach out between appointments. Quick check-ins can lead to timely interventions.
Tailored Dietary Approaches
A dietitian who specializes in mental health can make a significant difference. They can create meal plans that complement your medication regimen. For example, some patients on olanzapine find success with a low-carb diet to counteract the medication’s effects on insulin sensitivity.
Meal prepping is another effective strategy. Preparing balanced meals in advance can help you avoid impulsive food choices, especially during mood swings. This simple step often makes a big difference for many patients.
Exercise Routines for Bipolar Patients
Exercise is powerful for both weight management and mood stabilization. However, it’s important to tailor your routine to your energy levels, which can fluctuate with bipolar disorder.
During high-energy periods, activities like swimming or cycling can benefit you. These exercises burn calories without being too hard on your joints. During lower-energy phases, gentle yoga or short walks can help maintain activity levels without overwhelming you.
Consistency is key. Try to do 30 minutes of moderate activity most days of the week. If that seems daunting, start with 10-minute sessions and gradually increase.
Medication Adjustments and Alternatives
If weight gain persists despite lifestyle changes, discuss medication alternatives with your healthcare provider. For instance, if you’re on olanzapine and experience significant weight gain, switching to aripiprazole might help. A study found that maximum weight gain was seen with olanzapine treatment, while it was least with aripiprazole and ziprasidone.
Sometimes, adding a weight-neutral medication (like topiramate) can help offset weight gain from other medications. However, never adjust your medication without professional guidance.
Weight management is just one aspect of your overall treatment plan. The goal is to find a balance that keeps both your bipolar symptoms and weight in check. With the right strategies and support, it’s possible to manage your weight effectively while staying on track with your bipolar treatment.
Now that we’ve explored strategies for managing weight while on bipolar medication, let’s examine the psychological factors that can influence weight management for individuals with bipolar disorder.
The Mind-Body Connection in Bipolar Weight Management
Impact of Mood Swings on Eating Habits
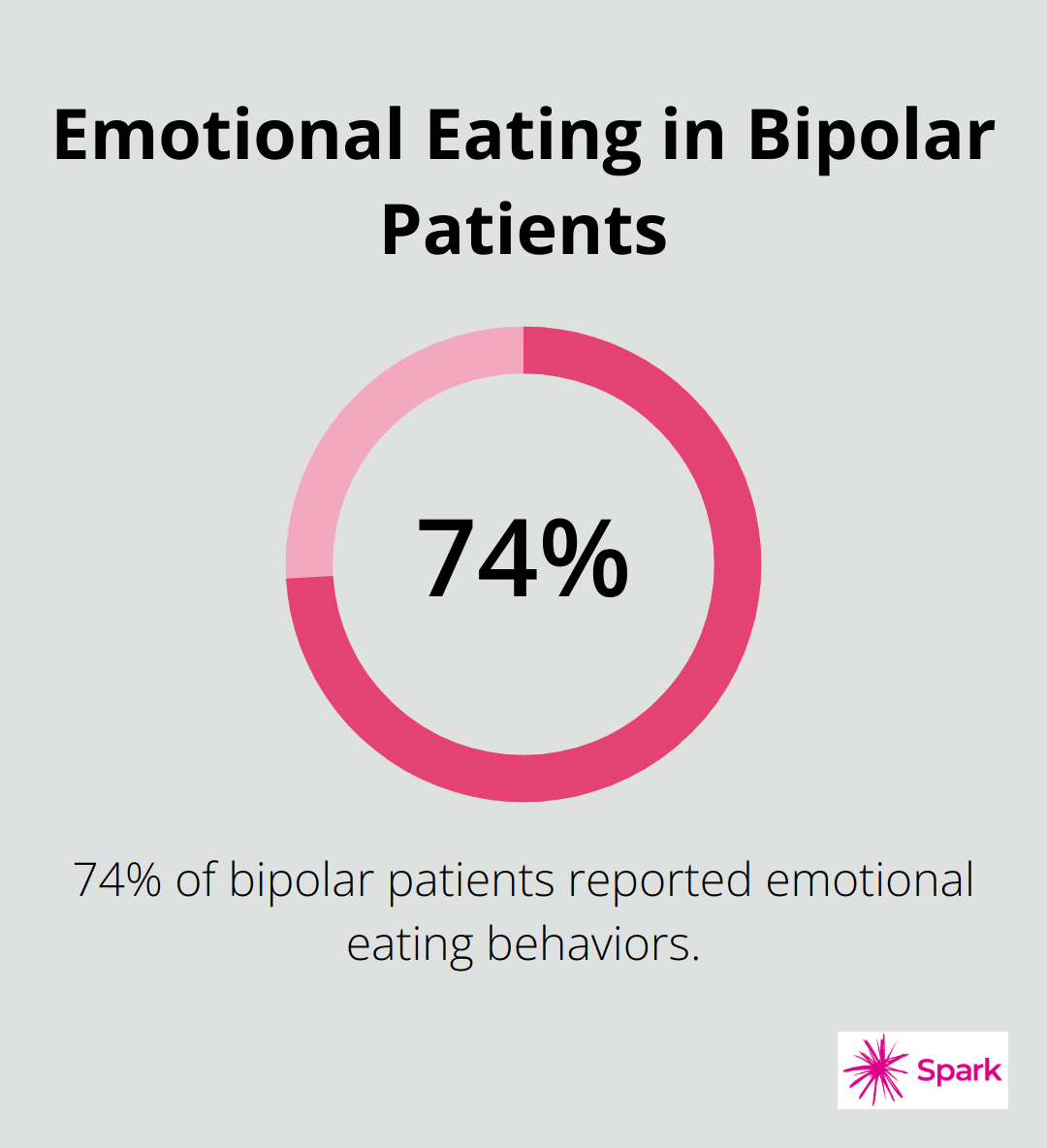
Bipolar disorder significantly affects eating patterns. Manic episodes often suppress appetite, while depressive phases can trigger overeating, particularly of high-calorie comfort foods. A study in the Journal of Affective Disorders revealed that 74% of bipolar patients reported emotional eating behaviors. Tracking mood and food intake helps identify these patterns and triggers.
Alternative Coping Strategies
Many individuals with bipolar disorder use food as a coping mechanism. This provides temporary relief but often leads to guilt and mood destabilization. Instead of comfort foods, try alternative strategies. Deep breathing exercises, progressive muscle relaxation, or a quick walk can manage emotions effectively. The goal is to find and establish personal coping methods that don’t involve food.
Cognitive Behavioral Techniques
Cognitive Behavioral Therapy (CBT) shows promise in helping bipolar patients manage their weight. CBT generally produces remission rates of 40% to 60% and robust improvements in eating disorder psychopathology, but it fails to produce weight loss.
Cognitive restructuring, a CBT technique, involves challenging negative thoughts about food and body image. For example, replace “I’ll never be able to lose weight” with “Weight loss is challenging, but I can make small, healthy changes every day.”
Behavioral activation schedules enjoyable, non-food-related activities during times when emotional eating is likely. This could include calling a friend or engaging in a hobby.
Building a Support Network
Long-term success in weight management often depends on a strong support system. This includes family, friends, healthcare providers, and support groups.
Online communities provide valuable support for people with bipolar disorder. These platforms offer a space to share experiences, tips, and encouragement with others who understand the unique challenges of managing bipolar disorder and weight (often more effectively than in-person groups).
Professional Guidance
Healthcare professionals play a vital role in managing the intersection of bipolar disorder and weight. Regular check-ins with a psychiatrist or therapist can help adjust treatment plans as needed. Nutritionists specializing in mental health can provide tailored dietary advice that complements medication regimens.
For those seeking comprehensive care, telepsychiatry services can provide convenient access to mental health professionals who understand the complexities of bipolar disorder and weight management.
Final Thoughts
Managing weight while on bipolar medication requires a personalized approach. Different medications impact weight differently, so patients must work closely with their healthcare providers to find the right balance. Regular monitoring, tailored dietary plans, and appropriate exercise routines form the foundation of effective weight management strategies.
Psychological factors play a significant role in bipolar medication weight loss efforts. Addressing emotional eating and developing healthy coping mechanisms are essential components of a comprehensive management plan. Cognitive behavioral techniques and building a strong support network can help individuals navigate the challenges of weight management while maintaining mental health stability.
We at Spark Healthcare offer telepsychiatry services to support individuals in managing bipolar disorder and associated weight concerns. Our team of mental health professionals understands the complexities of bipolar medication and weight management. We strive to provide individualized treatment plans that consider both mental health needs and weight management goals, helping patients achieve a balanced approach to their overall well-being.