Telepsychiatry has revolutionized mental health care, but prescribing controlled substances online comes with unique challenges. At Spark Mental Health, we’ve seen firsthand how this intersection of technology and medicine can impact patient care.
This blog post explores the complexities of telepsychiatry and controlled substances, covering regulations, benefits, risks, and best practices. We’ll provide you with essential information to navigate this evolving landscape in mental health treatment.
What Are Telepsychiatry and Controlled Substances?
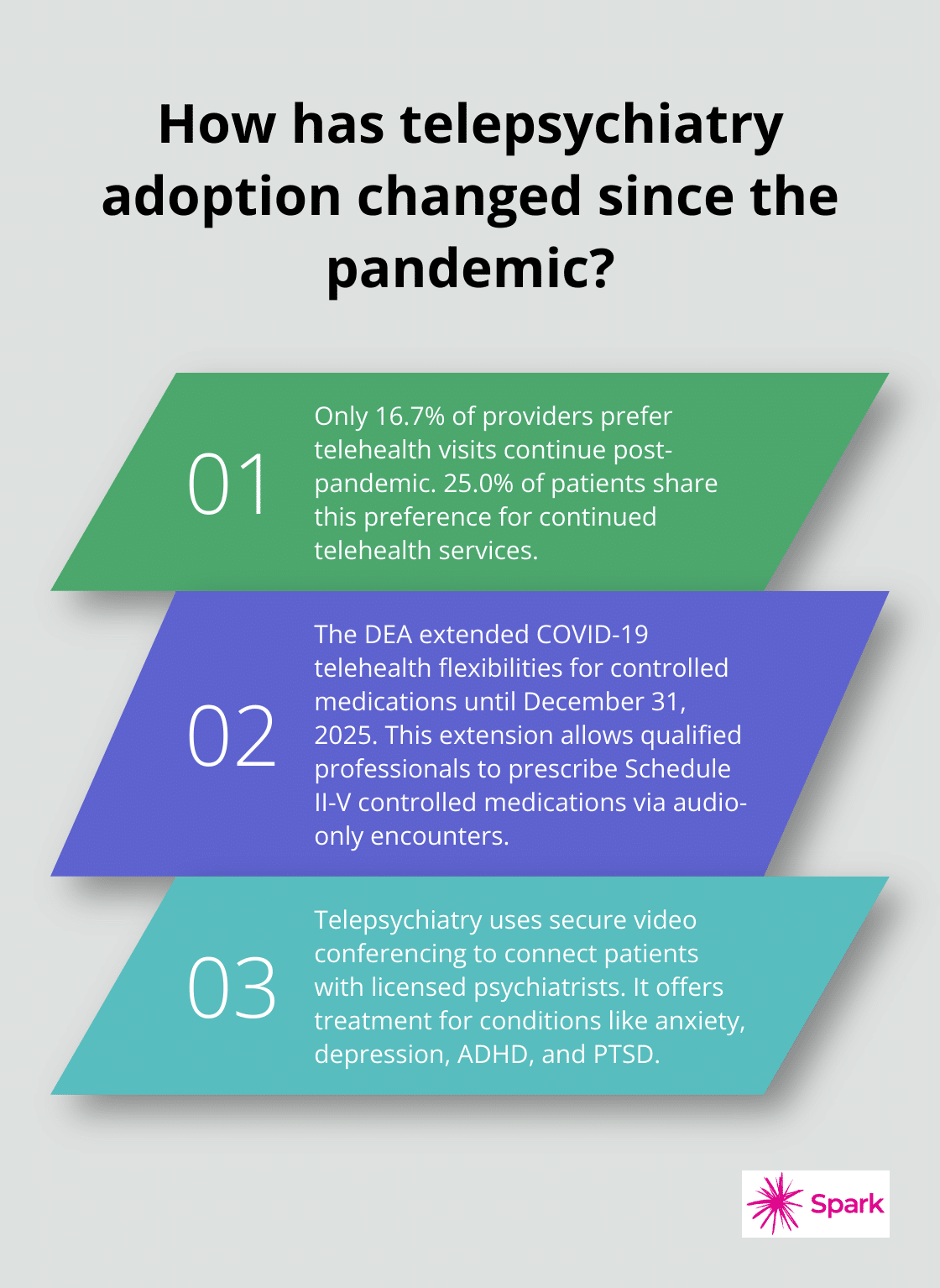
Defining Telepsychiatry
Telepsychiatry revolutionizes mental health care through digital platforms. It uses secure video conferencing to connect patients with licensed psychiatrists, offering treatment for conditions like anxiety, depression, ADHD, and PTSD. This approach has gained significant traction, though recent studies suggest that only 16.7% of providers and 25.0% of patients would prefer telehealth visits continue after the pandemic.
Understanding Controlled Substances
Controlled substances are medications that the government regulates due to their potential for abuse or dependence. These include stimulants for ADHD, benzodiazepines for anxiety, and certain pain medications. The prescription of these drugs via telepsychiatry remains a topic of ongoing debate and regulatory changes.
Current Regulations on Online Prescribing
As of November 2024, the DEA has extended COVID-19 telehealth flexibilities for controlled medications through December 31, 2025. This extension allows qualified professionals to prescribe Schedule II-V controlled medications via audio-only encounters, marking a significant shift from pre-pandemic norms.
However, regulations vary by state. Practitioners must adhere to state-specific rules when prescribing controlled substances via telepsychiatry. Some states may require an initial in-person evaluation before allowing telehealth prescriptions.
The Impact of Changing Regulations
The temporary nature of these extensions creates uncertainty for both providers and patients. The healthcare industry (including telepsychiatry providers like Spark Mental Health) must constantly monitor these changes to ensure their services remain compliant and accessible. These flexibilities have improved access to care, especially for patients in rural or underserved areas.
Ensuring Compliance and Safety
While current regulations allow for more flexibility, they also increase responsibility. Providers must document the medical necessity and rationale for prescribing controlled substances via telemedicine. This documentation maintains ethical standards and protects both patients and practitioners.
As we move forward, the intersection of telepsychiatry and controlled substance prescribing continues to evolve. The next section will explore the benefits and challenges this practice presents to both healthcare providers and patients.
The Double-Edged Sword of Online Prescribing
Breaking Down Barriers to Care
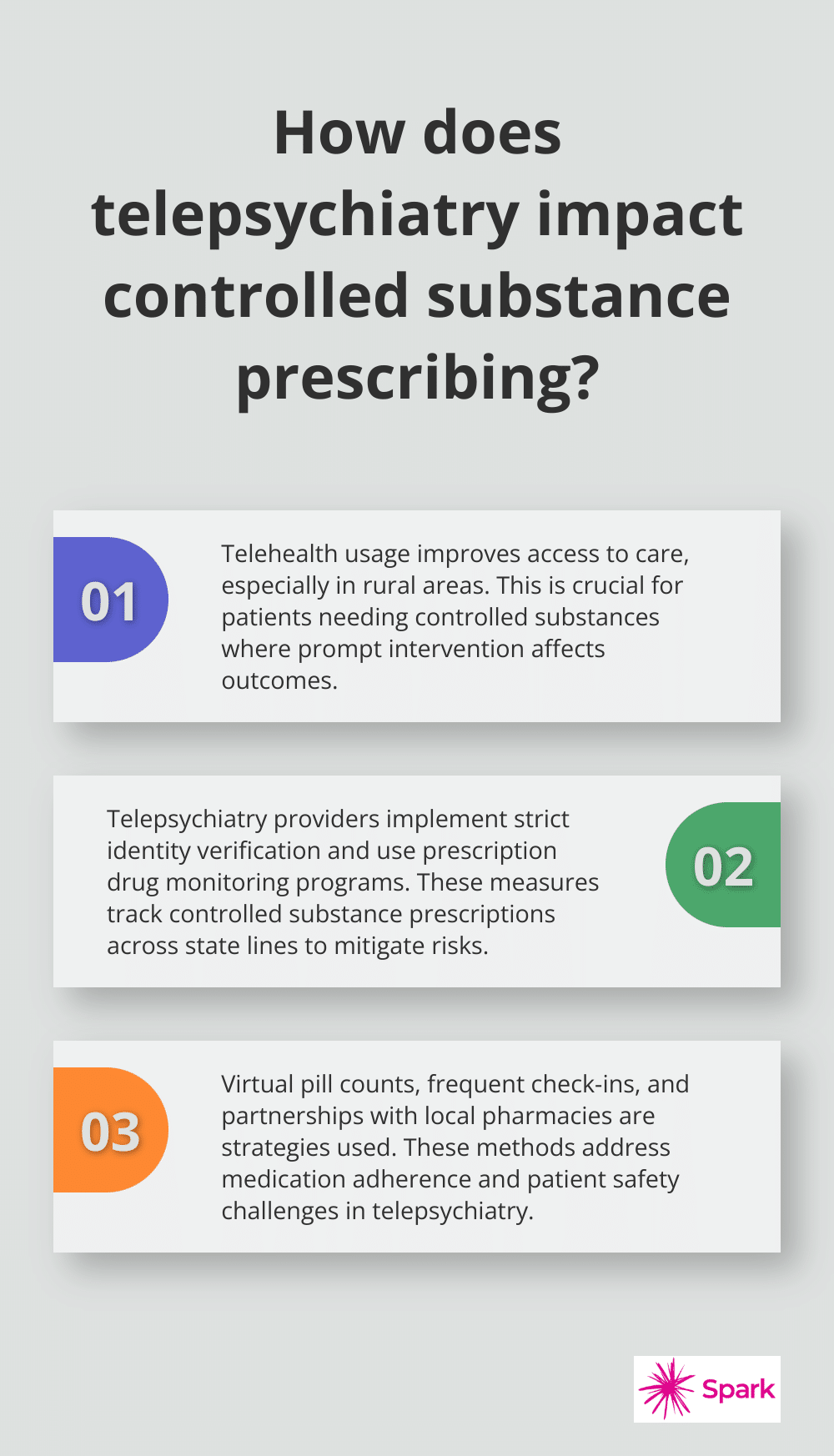
Telehealth usage has been promoted in all settings but has been identified as a panacea to issues of access and equity in the rural context. This improvement in access proves vital for patients who need controlled substances, where prompt intervention can significantly affect outcomes.
Risks of Virtual Prescribing
While improved access stands out as a clear advantage, online prescription of controlled substances carries potential risks. To combat this issue, telepsychiatry providers implement strict identity verification processes and use prescription drug monitoring programs (PDMPs) to track controlled substance prescriptions across state lines.
Patient Safety in a Virtual World
Medication adherence and patient safety present unique challenges in telepsychiatry. To address these concerns, telepsychiatry providers have developed strategies such as virtual pill counts, frequent check-ins, and partnerships with local pharmacies for medication delivery and monitoring.
Balancing Benefits and Risks
The practice of prescribing controlled substances via telepsychiatry requires a delicate balance. While it offers unprecedented access to care, it also demands heightened vigilance from providers. Telepsychiatry services (like Spark Mental Health) must continuously adapt their practices to maximize benefits while minimizing risks.
The Future of Online Prescribing
As technology advances and regulations evolve, the landscape of telepsychiatry and controlled substance prescribing will continue to change. Providers must complete an in-person evaluation by the telemedicine practitioner or another DEA-registered practitioner. The next section will explore best practices for telepsychiatry providers to ensure safe and effective care delivery in this dynamic environment.
How Telepsychiatry Providers Ensure Safe and Effective Care
Telepsychiatry providers face unique challenges when prescribing controlled substances online. Here’s how they deliver top-notch care in this evolving landscape.
Comprehensive Initial Evaluations
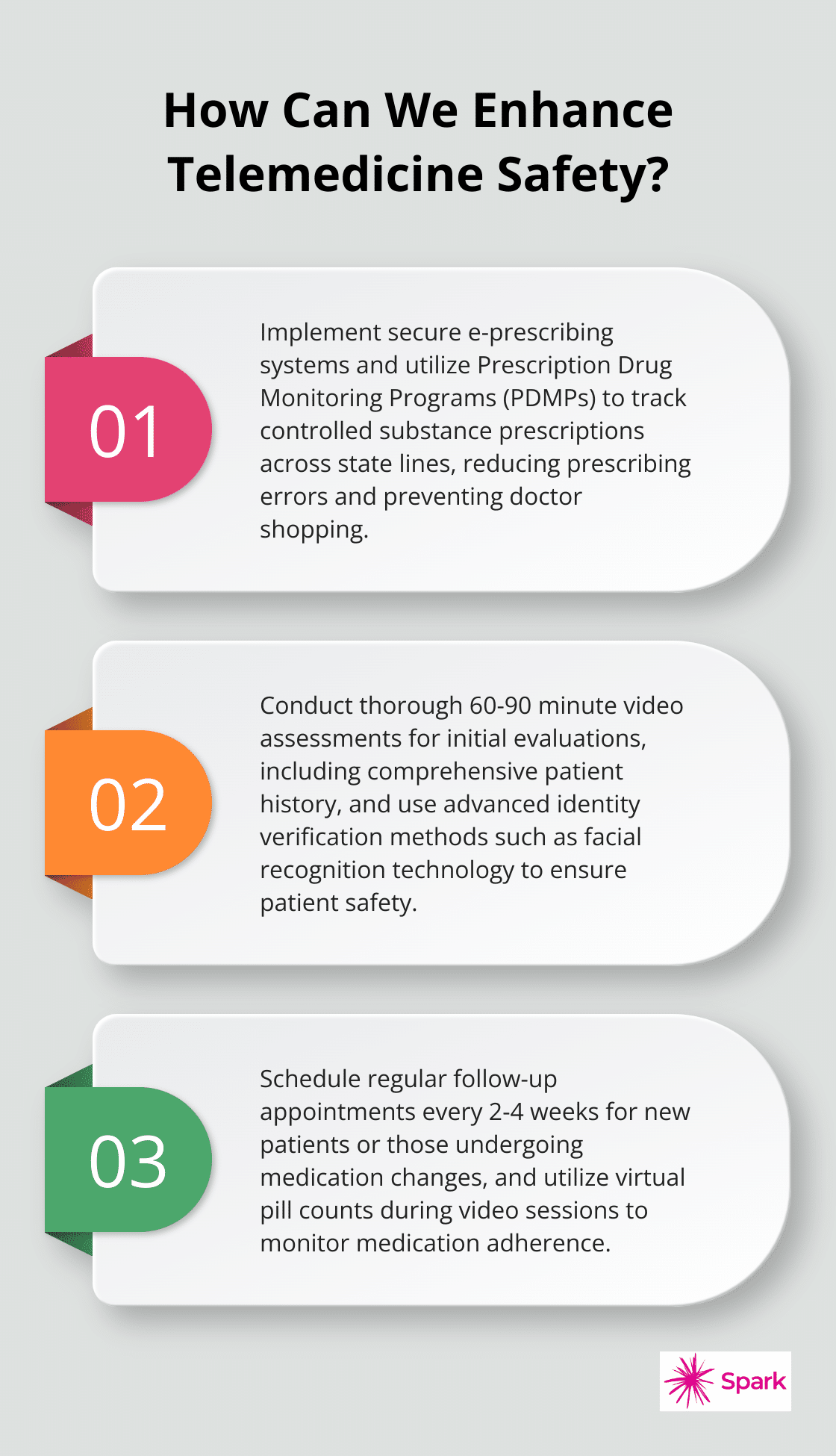
The foundation of effective telepsychiatry rests on thorough initial evaluations. Providers conduct extensive video assessments, which last 60-90 minutes, to gather a complete patient history. This includes past treatments, family history, and current symptoms. A study by the American Psychiatric Association found that 83% of patients felt their telepsychiatry evaluation was as thorough as in-person visits.

Providers must verify patient identity rigorously. This involves requesting government-issued ID and corroborating information with existing medical records. Some telepsychiatry platforms use advanced facial recognition technology to enhance security.
Secure Prescription Processes
Implementing secure prescription processes is essential when dealing with controlled substances. Electronic prescribing (e-prescribing) systems have become the gold standard, reducing prescribing errors, increasing efficiency, and helping to save on healthcare costs.
Providers also utilize Prescription Drug Monitoring Programs (PDMPs) to track controlled substance prescriptions across state lines. This helps prevent doctor shopping and identifies potential substance abuse issues. Emerging evidence supports that the implementation of state PDMPs reduces opioid prescriptions, opioid diversion, and supply.
Continuous Monitoring and Treatment Adjustments
Effective telepsychiatry doesn’t stop with the initial evaluation and prescription. Ongoing monitoring is vital, especially for patients on controlled substances. Providers schedule regular follow-up appointments, typically every 2-4 weeks for new patients or those undergoing medication changes.
Virtual pill counts help ensure medication adherence. Patients show their medication bottles to the camera during video sessions, allowing providers to track usage. Some telepsychiatry services explore partnerships with smart pill bottles that automatically track and report medication use.
Providers adjust treatment plans based on patient progress and feedback. This might involve changing medication dosages, switching to alternative treatments, or incorporating additional therapeutic approaches like cognitive-behavioral therapy.
Professional Development
Telepsychiatry providers must stay informed about the latest research and guidelines in their field. Per the Ryan Haight Act, the prescribing practitioner is required to have conducted one in-person medical evaluation with the patient before prescribing via telemedicine.
These best practices allow telepsychiatry providers to offer safe, effective, and accessible mental health care, even when prescribing controlled substances. As the field continues to evolve, ongoing adaptation and commitment to patient safety remain paramount.
Final Thoughts
Telepsychiatry has revolutionized mental health care, offering unprecedented access to treatment, including the prescription of controlled substances. The extended flexibilities for prescribing controlled medications via telehealth until December 31, 2025, have improved care accessibility, especially for underserved areas. However, these advancements require providers to navigate complex regulations, implement robust security measures, and maintain high standards of patient care.
The landscape of telepsychiatry and controlled substance prescribing will continue to evolve. We expect further technological advancements, potentially including AI-driven diagnostic tools and more sophisticated medication tracking systems. The human element of care will remain irreplaceable, as ongoing dialogue between healthcare professionals, policymakers, and patients shapes the future of telepsychiatry controlled substances.
At Spark Mental Health, we provide high-quality, accessible mental health care through telepsychiatry. Our approach combines evidence-based practices with the latest technological advancements to ensure safe, effective treatment for conditions like anxiety, depression, ADHD, and PTSD. The goal remains clear: to harness the power of technology to improve mental health outcomes while maintaining the highest standards of patient care and safety.