Depression treatment has come a long way in recent years. At Spark Mental Health, we’re excited to explore novel depression treatments that offer hope to those who haven’t found relief through traditional methods.
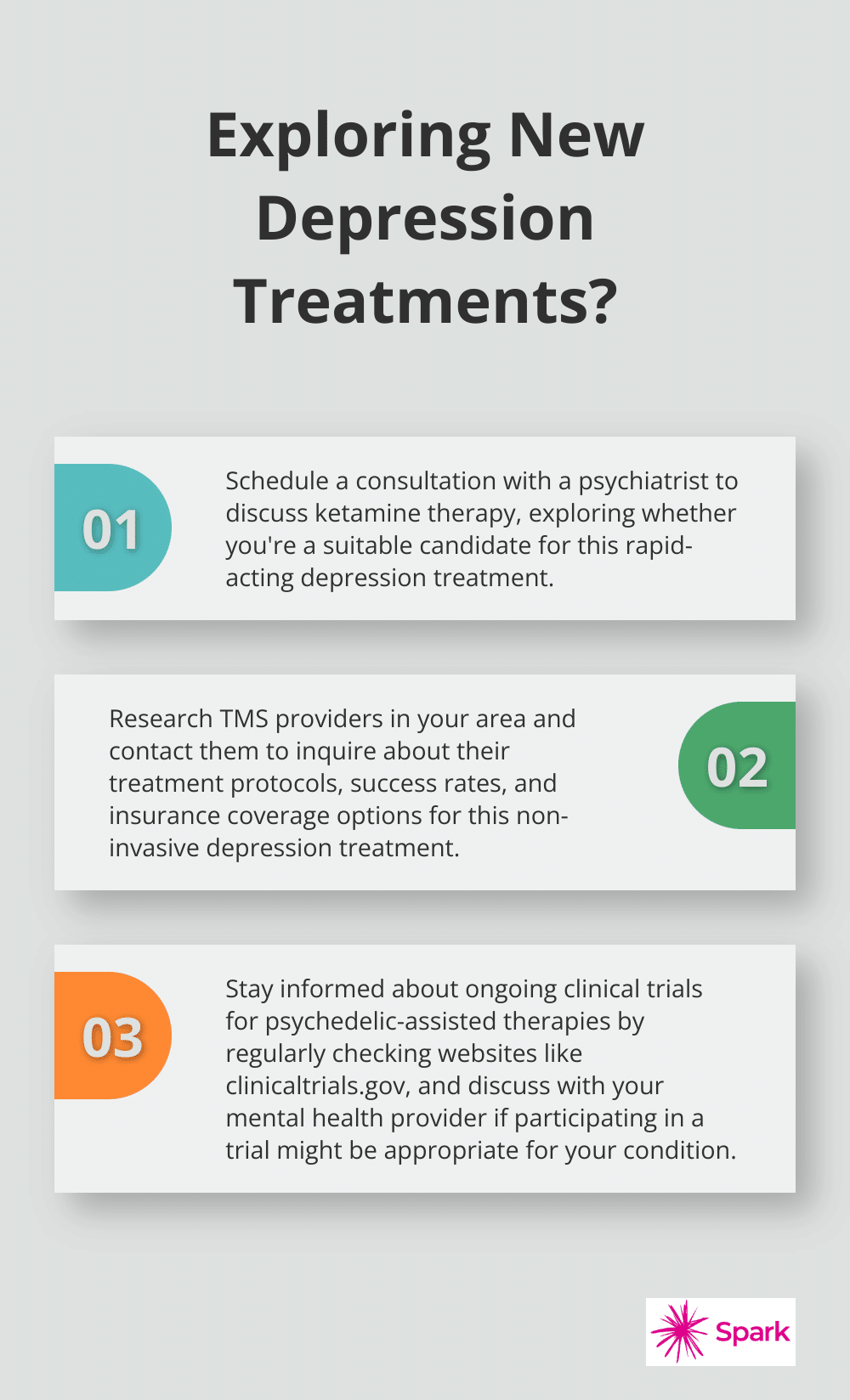
From ketamine therapy to transcranial magnetic stimulation and psychedelic-assisted therapy, these innovative approaches are changing the landscape of mental health care. In this post, we’ll dive into these cutting-edge treatments, their potential benefits, and what you need to know about accessing them.
Ketamine: A Rapid-Acting Depression Treatment
Ketamine therapy has revolutionized depression treatment, offering new hope to patients who haven’t responded to traditional antidepressants. This anesthetic, originally used in medical procedures, has demonstrated remarkable potential in rapidly alleviating depressive symptoms.
The Mechanism of Ketamine
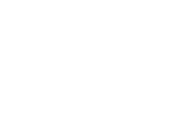
Unlike conventional antidepressants that target serotonin, ketamine acts on the glutamate system in the brain. It blocks NMDA receptors, which leads to increased production of proteins that form new neural connections. This process (known as synaptogenesis) can improve mood and cognitive function within hours or days, rather than the weeks or months typical of standard antidepressants.
Benefits and Potential Risks
The most striking benefit of ketamine is its rapid action. Many patients report significant mood improvements within 24 hours of treatment. A study published in the American Journal of Psychiatry found that 50–70% of patients with treatment-resistant depression showed a positive response to ketamine therapy.
However, ketamine isn’t without risks. Common side effects include dizziness, nausea, and dissociation during treatment. Long-term risks are still under investigation, but potential concerns include bladder problems and cognitive impairment with prolonged use. It’s important to weigh these factors carefully with a healthcare provider.
Treatment Protocols
Ketamine therapy typically involves a series of infusions or intranasal treatments. Both intravenous (IV) ketamine infusions and esketamine nasal spray (Spravato, FDA-approved for treatment-resistant depression) are available treatment options.
IV ketamine treatments usually consist of 6 initial infusions over 2-3 weeks, followed by maintenance treatments as needed. Each session lasts about 40 minutes, with patients monitored for 1-2 hours afterward. Esketamine is administered twice weekly for the first month, then weekly or bi-weekly thereafter.
Comprehensive Approach
Ketamine therapy should be part of a comprehensive treatment plan. Combining it with psychotherapy and lifestyle interventions often yields optimal results. Patients must undergo careful screening and monitoring throughout treatment.
While ketamine offers exciting possibilities, it’s not suitable for everyone. Factors like medical history, current medications, and specific mental health conditions can affect eligibility. A thorough evaluation by a qualified psychiatrist is essential before starting treatment.
As we explore innovative depression treatments, it’s important to consider other emerging options. One such treatment that has gained attention in recent years is Transcranial Magnetic Stimulation (TMS). Let’s examine how this non-invasive technique is changing the landscape of depression treatment.
Transcranial Magnetic Stimulation (TMS): A Non-Invasive Approach to Depression Treatment
Transcranial Magnetic Stimulation (TMS) represents a significant advancement in depression treatment. This non-invasive brain stimulation technique offers hope to patients who haven’t responded well to traditional antidepressants.
The Science Behind TMS
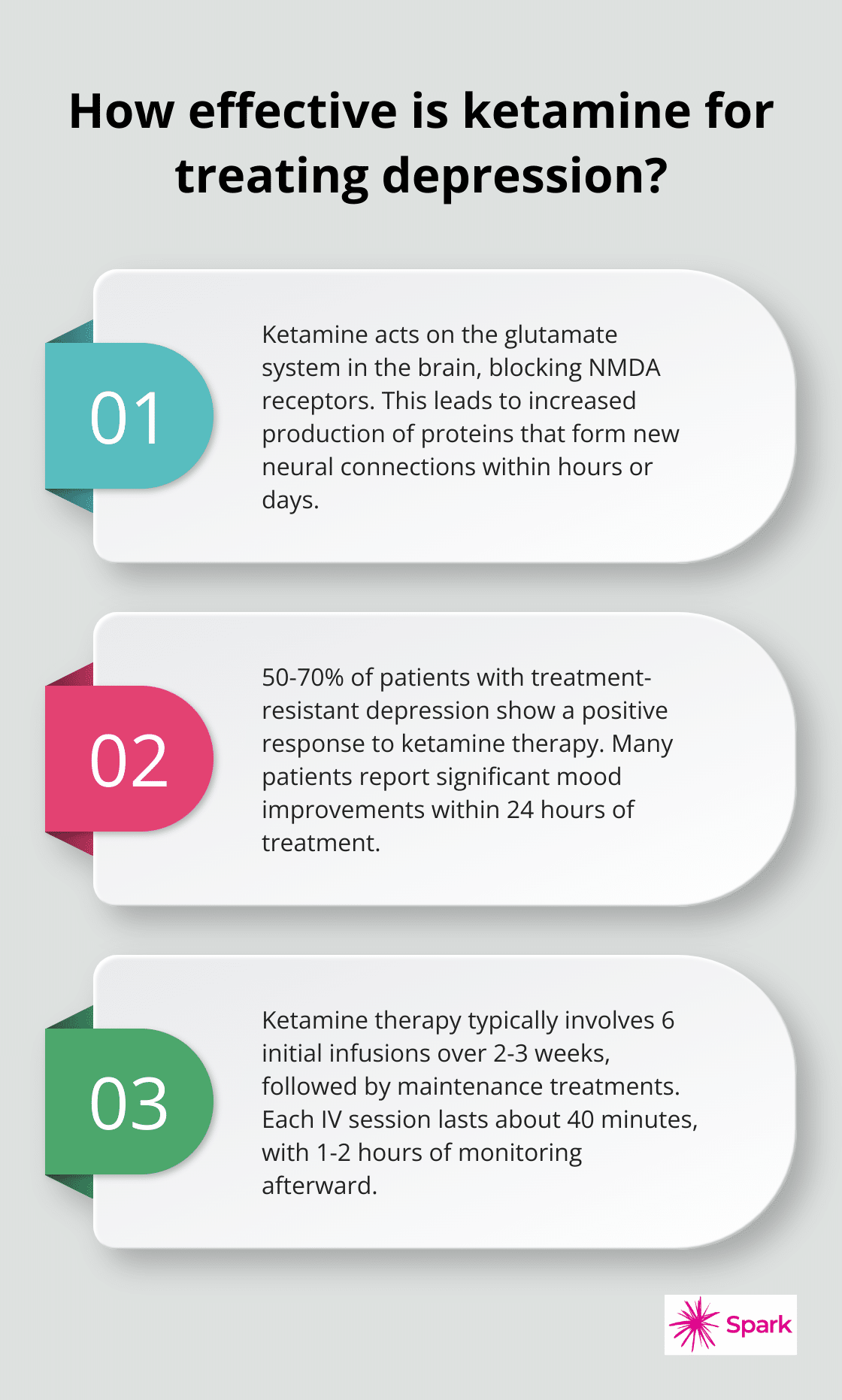
TMS uses magnetic fields to stimulate specific brain areas associated with mood regulation. The treatment targets the dorsolateral prefrontal cortex, a region often underactive in people with depression. Repeated activation of this area can help normalize brain activity and alleviate depressive symptoms.
A recent study found that the effectiveness of rTMS has previously been observed as quite variable, with reported response rates ranging from 30-60%.
The TMS Treatment Process
TMS sessions typically last about 40 minutes and take place on an outpatient basis. Patients remain awake and seated comfortably during treatment. A medical professional places a magnetic coil against the scalp, which delivers brief magnetic pulses to the target brain area.
Most patients require 5 sessions per week for 4-6 weeks (totaling 20-30 sessions). Some individuals may benefit from maintenance sessions after the initial treatment course.
Side Effects and Considerations
TMS boasts a relatively mild side effect profile compared to many antidepressant medications. The most common side effects include:
- Scalp discomfort at the stimulation site
- Headaches (which usually subside after the first few sessions)
It’s crucial to note that TMS isn’t suitable for everyone. Patients with metal implants in or near the head (such as cochlear implants or aneurysm clips) generally can’t undergo TMS due to the strong magnetic fields involved.
Combining TMS with Other Treatments
While TMS shows great promise, it’s just one tool in the arsenal against depression. Many mental health professionals recommend a comprehensive approach to care. This often involves combining TMS with other evidence-based treatments like psychotherapy and medication management for optimal results.
As research continues, the potential of TMS to offer relief to those struggling with depression grows more exciting. If you’re considering TMS, a qualified mental health professional can help determine if it’s the right option for you and guide you through the treatment process.
The landscape of depression treatment continues to evolve, with innovative approaches emerging alongside established therapies. One particularly intriguing area of research involves the use of psychedelics in treating depression. Let’s explore how substances like psilocybin and MDMA are reshaping our understanding of mental health treatment.
Psychedelics in Depression Treatment: A New Frontier
Psilocybin: Nature’s Antidepressant?
Psilocybin, the active compound in “magic mushrooms,” stands at the forefront of psychedelic research for depression. A study published in the New England Journal of Medicine revealed that psilocybin at a single dose of 25 mg, but not 10 mg, reduced depression scores significantly more than a 1-mg dose over a period of 3 weeks.
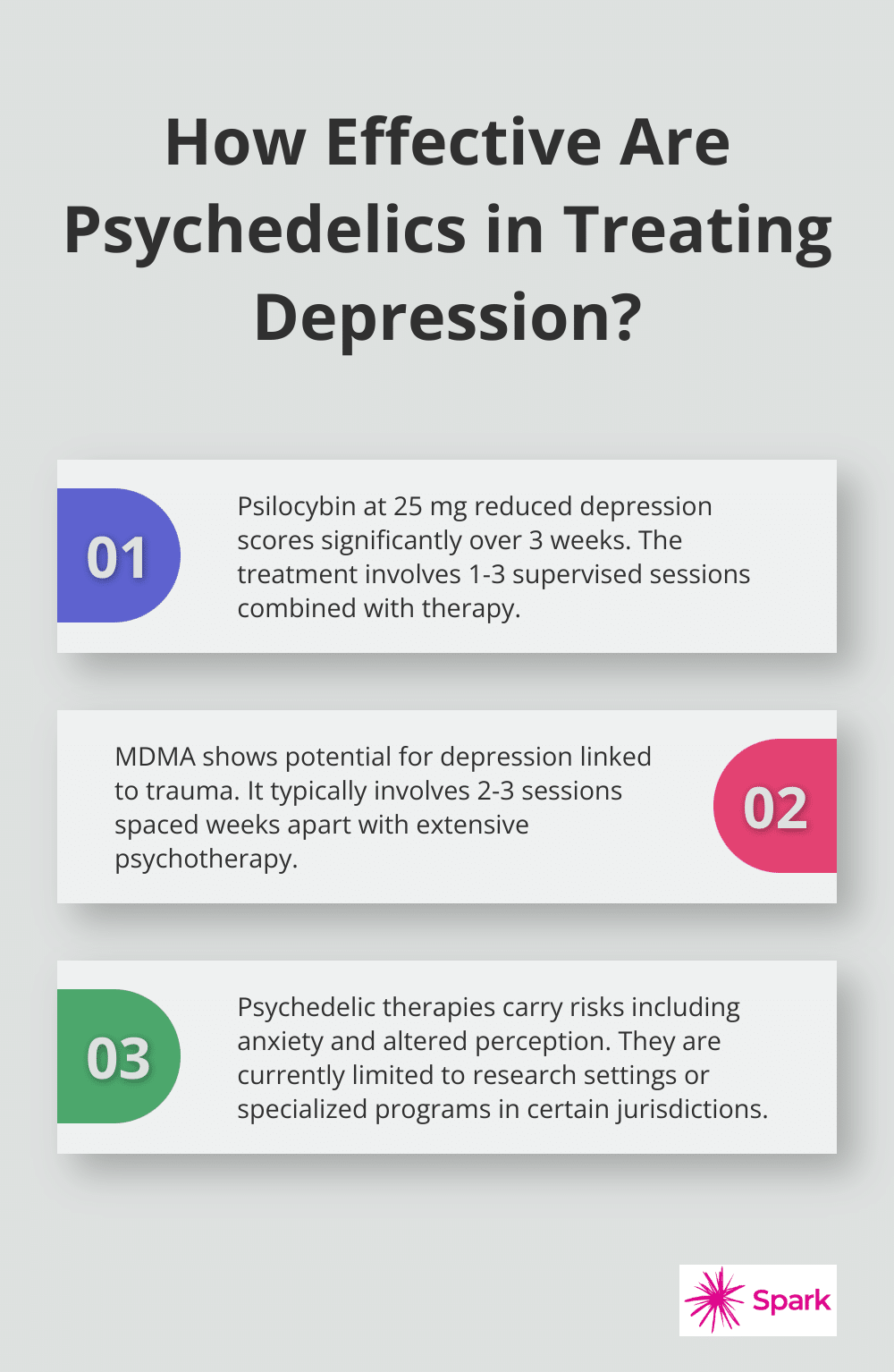
The treatment protocol usually involves one to three sessions where patients receive a carefully measured dose of psilocybin under medical supervision. These sessions combine with preparatory and integration therapy to maximize benefits and minimize risks.
MDMA: Healing Trauma and Depression
MDMA (commonly known as ecstasy) shows potential in treating depression, particularly when linked to trauma. MDMA-assisted therapy is currently under investigation for safety and efficacy. It is not yet approved by the FDA and does not work for everyone.
MDMA therapy typically involves 2-3 sessions spaced several weeks apart, with extensive psychotherapy before and after each session. This approach creates a window of increased emotional openness, allowing patients to process traumatic memories more effectively.
Navigating Risks and Regulations
While promising, psychedelic therapies come with potential risks. These can include temporary anxiety, altered perception, and in rare cases, exacerbation of underlying mental health conditions. It’s essential that trained professionals administer these treatments in controlled settings.
As of 2025, psilocybin and MDMA remain classified as Schedule I substances in the United States, limiting their use to research settings. However, several states and cities have decriminalized or legalized these substances for therapeutic use. Oregon, for example, has established a state-licensed psilocybin therapy program.
Patients interested in psychedelic-assisted therapy should know that access is currently limited to clinical trials or specialized programs in certain jurisdictions. The FDA has granted breakthrough therapy designation to both psilocybin and MDMA, potentially fast-tracking their approval for depression and PTSD treatment, respectively.
Current Availability and Future Prospects
While psychedelic-assisted therapies show promise, they are not yet widely available for depression treatment. Many mental health providers (including Spark Mental Health) do not currently offer these therapies due to regulatory restrictions and ongoing research. However, patients can explore other innovative treatments for treatment-resistant depression like ketamine therapy and TMS, which are more readily accessible and have established safety profiles.
As research progresses, the landscape of depression treatment continues to evolve. Patients should consult with qualified mental health professionals to explore all available options and determine the best treatment plan for their unique needs.
Final Thoughts
Novel depression treatments expand the horizons of mental health care. From ketamine’s rapid-acting effects to TMS’s non-invasive approach and psychedelic-assisted therapies’ potential, these innovative options offer new hope for those struggling with depression. However, these treatments are not one-size-fits-all solutions, and their effectiveness can vary greatly from person to person.
Professional guidance and personalized care are essential components of any treatment plan. A qualified mental health professional can assess individual needs, medical history, and specific circumstances to determine the most appropriate course of action. Ongoing research continues to uncover new insights into depression’s complexities and potential therapeutic approaches.
At Spark Mental Health, we offer personalized, evidence-based telepsychiatry services for conditions including depression. Our team of professionals creates individualized care plans that may incorporate innovative therapies alongside traditional approaches (ensuring comprehensive and effective treatment). We provide access to expert care from the comfort of your home.